Early Fertility Trials of Semen Collection Device Previously Demonstrated to Improve Semen Parameters and Pregnancy Rates in Animal Models
Authors
Robert Kaufmann1, Lisa Welch3, Samuel Prien2, Jennifer Phy2
- Department of Obstetrics and Gynecology, Texas Tech University Health Sciences Center, Amarillo, TX
- Department of Obstetrics and Gynecology, Texas Tech University Health Sciences Center, Amarillo, TX
- Department of Animal and Food Sciences, Texas Tech University, Lubbock, TX
Publications
Fertility and Sterility Vol. 98, Issue 3 Supplement S249. Published in issue: September 2012 – poster presentation.
Objective
It is well documented that sperm are susceptible to shock during processing which often induces biochemical pathways leading to cell death. Previous animal studies from this lab suggest a modification of the collection technique (Device for Improved Semen Collection; DISC) can prevent activation of these pathways, yielding larger, more motile pools of sperm for treatment and resulting in higher pregnancy rates. The objective of the present study was to evaluate the DISC in humans.
Design
Lab-based trials in donors and infertility patients.
Materials and Methods
Donors collected in a standard specimen cup (SSC) and the DISC. The samples were then processed and cultured for 24 hours. Aliquots were taken, over time, for semen analysis using CASA, and biochemical assessment, including: acrosomal status, lipid peroxidation, mitochondrial membrane potential (MMP) and DNA damage. A preliminary clinical trial was then conducted comparing the DISC to SSC. Couples undergoing IUI alternated semen collections between the DISC and SSC for up to 6 cycles
Results
Donor samples collected in the DISC exhibited improved semen parameters when compared to the SSC: viability (p < 0.005), motility rates (p = 0.066), path velocities (p = 0.061), progressive velocity (p < 0.05), and motility index (p < 0.034). Further, cells collected in the DISC had more intact acrosomes (p < 0.017) and retained higher MMP (p < 0.004). 24 couples completed 51 IUI cycles (26 SSC vs. 25 DISC). As in the donor trial, samples from the DISC trended to have higher motility (p = 0.063) and progressive velocity (p = 0.057). There were 9 pregnancies (17.6%) with equivalent results in the DISC vs. SSC, 4 vs. 5 (p = 0.762). However, while 100% of the pregnancies in the DISC delivered, only 40% in the SSC did (p = 0.058).
Conclusions
As in the animal studies, results suggest improved semen quality from the DISC. Larger numbers are needed to determine if improved semen quality will lead to the increased pregnancy rates seen in other species.
Supported By
TTU Office of Commercialization.
Figure 1
Rate of Post-Wash Sample Recovered Motility
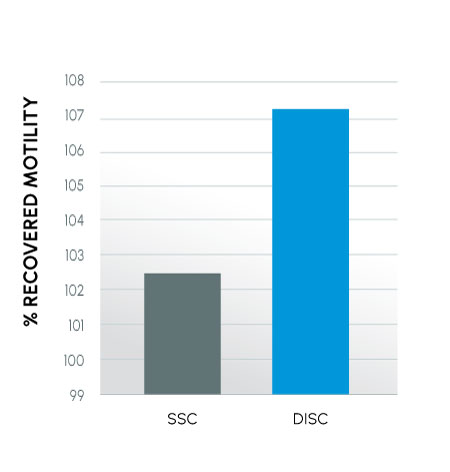
A total of 51 cycles were completed by 24 couples recruited from two fertility centers and randomized. 25 cycles were measured in the DISC and 26 in the SSC. The rate of post-wash sample recovered motility (% of post-wash motility / % pre-wash motility) reflects how many motile cells per mL are present after washing.
Insights
Knowing that both the protective properties of ProteX and the addition of media yield biochemically and physiologically healthier sperm, researchers naturally questioned if healthier sperm result in healthier pregnancies. A very small trial of 24 patients was undertaken to evaluate if ProteX is equivalent to standard collection methods.
While there is often an expected lift in motility after washing sperm, there is no benchmark for recovered motility. It was found that across all patients, 5% more motile sperm were recovered post-wash when patients used ProteX. While this may seem like a small percentage, a 5% increase may be of relative significance as we look at healthy pregnancies and live births (FIGURE 2)
Figure 2
Rate of Post-Wash Sample Recovered Motility
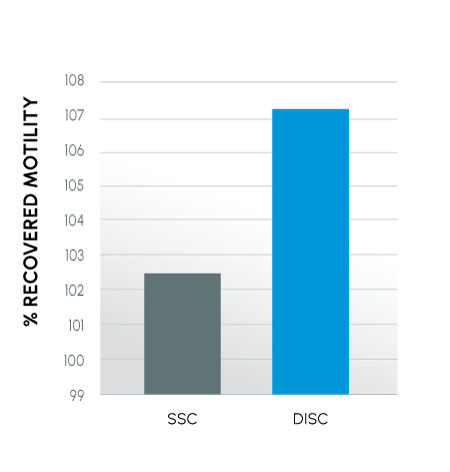
Conception rates (p = 0.83) and live births (p < 0.02) from semen collected in a standard specimen cup (SSC) versus a new device for improved semen collection (DISC)
Insights
As expected with this sample size, there was no statistical difference in conception rate. What was not expected by the team was that while over half of the patients who conceived using the standard cup experienced a miscarriage, all patients who conceived using ProteX had a baby come to full term, suggesting that healthier sperm result in more live births
Direct insights into the research, methodology, and results have been added to this summary by the co-inventors themselves. This additional information is intended to provide helpful context to professional practitioners and does not fundamentally change the outcomes or interpretation of the published results. All ProteX research content and material is the property of Reproductive Solutions and may not be redistributed or republished without our consent. All rights reserved.
All Scientific Studies
Sample. Test. See for yourself.
Compare ProteX to the standard specimen cup with our sterile sample kit.