Studies
A Retrospective Review of IUI Clinical Outcomes Following Semen Collection in the ProteX versus a Standard Specimen Cup
Preliminary Clinical Outcomes in an IVF Program using the ProteX versus a Standard Specimen Cup for Semen Collection
Early Fertility Trials of Semen Collection Device Previously Demonstrated to Improve Semen Parameters and Pregnancy Rates in Animal Models
Pregnancy Trials Using the Device for Improved Semen Collection
Physiological and Biochemical Assessment of a New Semen Collection Device
Continued Evaluation of a New Semen Collection Technique / Container in Subfertile and Infertile Individuals Using a Cross-species Model
New Semen Collection Technique / Container Improves Semen Quality
Improving Semen Quality Using a Modified Collection Technique
A Novel Collection Technique for Improved Semen Quality
Improvement of the Semen Collection Environment Using a New Semen Collection Device
ProteX Original Research | Human Study
New Semen Collection Technique / Container Improves Semen Quality
Authors
- Department of Animal and Food Sciences, Texas Tech University, Lubbock, TX
- Department of Obstetrics and Gynecology, Texas Tech University Health Sciences Center, Lubbock, TX
Publication
Objective
To date, the common thread in the use of semen collection / extension techniques, whether being used for intrauterine insemination, cryopreserved semen, or advanced reproductive techniques such as in vitro fertilization, is that the samples are collected into a dry, unprotected specimen container. This container, by its nature, allows for drastic shifts in temperature and pH resulting in damage to the spermatozoa.
Previous studies in the canine and limited studies in humans have shown that collecting semen into a modified collection vessel containing a warmed, osmotically balanced media, semen parameters can be improved by lessening cold and pH shock upon collection. The objective of this study was to determine if the use of this new semen collection technique / container would yield similar improvements in semen parameter in the human as compared to the traditional collection container.
Design
The study was designed as a Latin Square to account for the variations between collections within the same donor and subjects were randomized by first collection.
Materials and Methods
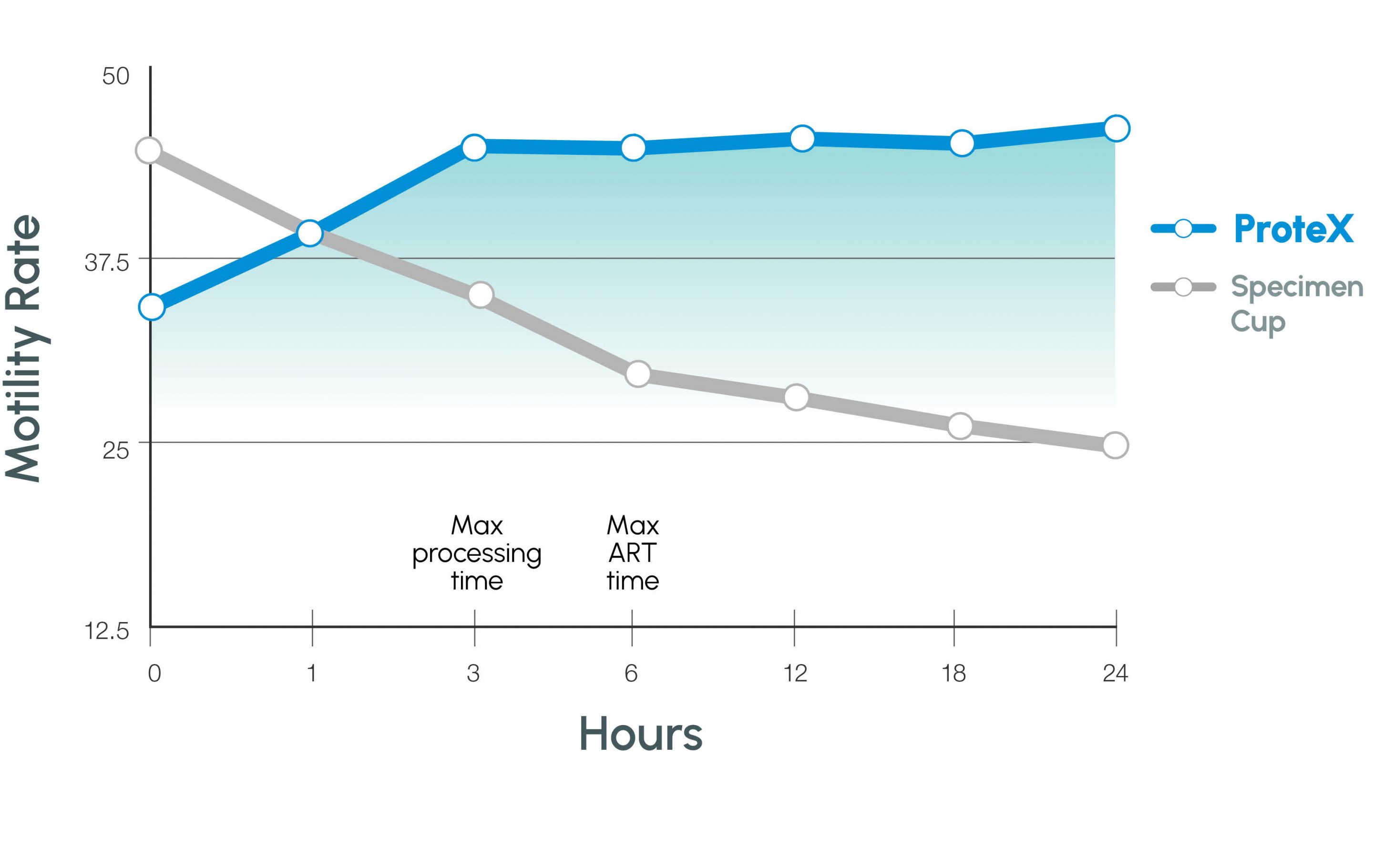
Twelve donors provided three semen samples each to be used in three separate treatments. The control samples (Treatment I) were collected into a standard, dry specimen container. Treatment II and III samples were collected into a modified specimen container that allowed the sample to be funneled into an insulated, reduced volume center well containing 1 mL of pH-buffered media. In the case of Treatment II, the media was at 37°C, while the media in Treatment III was held at room temperature (23°C). After collection, the samples were held at 37°C and allowed to liquefy before processing using a standard semen washing technique. The samples were then placed into 5 mL of fresh media and maintained in a 37°C, 5% CO2 incubator at 95% relative humidity. Standard semen parameters and biochemical markers were evaluated at 0, 1, 3, 6, 12, 18, and 24 hours post-processing. Data analysis was performed with SPSS using the general linear model and appropriate t-tests.
Results
Conclusions
Modification of the semen collection technique / container resulted in improved semen parameters for extended time periods post-collection. The data suggests the new technique can yield significantly more motile sperm by placing the sample into a physiologically favorable environment (eliminating pH and cold shock), thus making more sperm available for use in a variety of infertility treatments. The improvement in semen parameters over time as seen in both treatments may lead to improved patient care by allowing the patient to collect at home while maintaining superior semen quality.
Figure 1
Motility at 24 hours with container and media / temperature variables
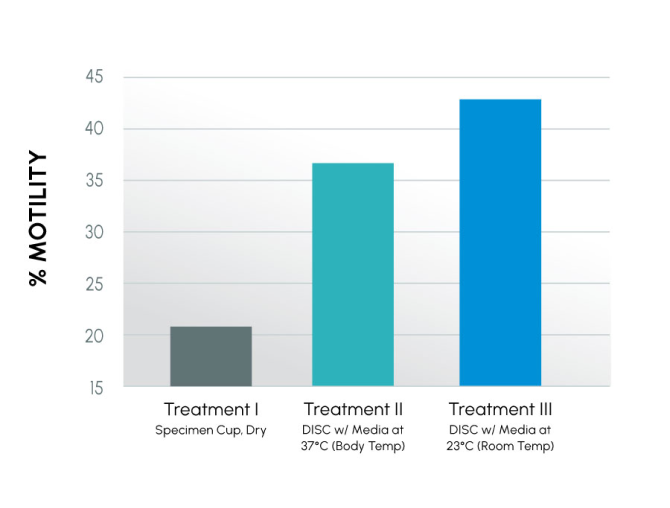
Figure 2
Motility PROGRESSION COMPARISON
Insights
In this study, it was confirmed that room temperature media improved semen parameters the most. By using room temperature media, the semen sample was allowed to drive the temperature change vs. the outside environment. Motility at 24 hours for these three treatments is different from the previous study due to differences in the human samples. However, the delta between Control and DISC(s) is similar between studies.
Direct insights into the research, methodology, and results have been added to this summary by the co-inventors themselves. This additional information is intended to provide helpful context to professional practitioners and does not fundamentally change the outcomes or interpretation of the published results. All ProteX research content and material is the property of Reproductive Solutions and may not be redistributed or republished without our consent. All rights reserved.
